Chapter 31 Review Answers Principles of Radiographic Imaging 6th Edition
Image Wisely is a joint initiative of the American College of Radiology, Radiological Society of North America, American Society of Radiological Technologists and American Association of Physicists in Medicine.
- Home
- Computed Tomography
- How to Understand and Communicate Radiation Risk

How to Understand and Communicate Radiation Risk
Donald J. Peck, PhD, Henry Ford Health System, Detroit, MI
Ehsan Samei, PhD, Duke University Medical Center, Durham, NC
Updated March 2017 | Download PDF

Many medical imaging examinations involve exposure to ionizing radiation. The exposure amount in these exams is very small, to the extent that the health risk associated with such low levels of exposure is frequently debated in scientific meetings. Nonetheless, the prevailing scientific view is that there is a finite (though small) amount of risk involved with such exposures. The risk is increased with the amount of exposure, repeated exposures, and when the patient is young. This material aims to provide a brief overview of the risk associated with medical imaging examinations that involve ionizing radiation.
A. Radiation Biology Review
Ionizing radiation can cause tissue damage. Tissue damage occurs through the change in chemical properties of molecules in the tissue following exposure to radiation. The major contributor to damage from radiation is through radiation changing a water molecule into a new form called a "free radical". Free radicals are chemically highly active and as such can have reactions with genetic molecules of the cell (i.e., the DNA). This can cause damage to the DNA most of which is readily repaired by the cell. If it is not, it can result in cell death. Alternatively, if the DNA damage is repaired erroneously, it can result in an alteration of the genetic encoding leading to hereditary changes or cancer induction.
Changes that result in cell death are termed "Deterministic Effects"; while changes to the DNA encoding that lead to other adverse changes are termed "Stochastic Effects" (see Figure 1).
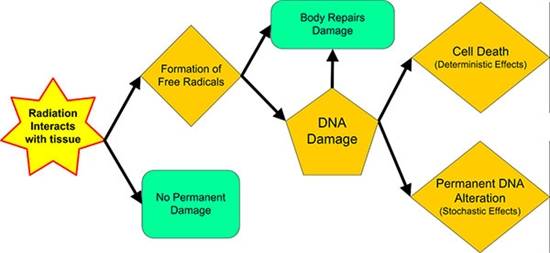
Figure 1. Radiation – Deterministic and Stochastic Effects
A.1. Deterministic Effects (Cell Death)
Cells are dying all of the time in the body from physical, chemical and other causes (i.e. "natural causes"). In most cases these cells are replaced or the body adapts to function normally when this occurs. But if too many cells die, the damage caused may not be compensated for very easily. Whether the organ can continue to function depends on how much of the organ is damaged and the number of cells within the organ that are damaged. This is due to the structure of tissues and organs into functional subunits (FSU). A FSU is a set of tissues or organs whose ultimate function is dependent on the overall workings of each subunit, e.g. proper digestion of food requires the entire digestive tract to function properly – stomach, intestines, etc. But when the tissue or organ has parallel functional structure, rather than in series like the digestive tract, damage from any source can be compensated for more easily and normal function can be maintained. Therefore, whole organ irradiation or irradiation of an entire FSU reduces or eliminates the ability of a tissue or organ to be repaired. Yet if some part of the FSU is left unexposed, partial function can continue and repair of the damage may be possible.
Deterministic effects can be thought of as effects in which the outcome can be determined, i.e. they are predictable. Deterministic effects will occur if the radiation deposits enough energy in tissue to disrupt the tissue's FSU enough. The amount of energy required to cause these changes is different for different tissues and this amount of radiation is called the threshold dose for tissue damage.
Deterministic effects are usually divided into tissue specific/local changes and whole body effects. Examples of tissues that are known to demonstrate deterministic effects from radiation exposure are:
- Tissue specific damage from radiation
- Lens of the eye
- Detectable opacities
- Cataract formation
- Skin
- Skin reddening (erythema)
- Hair loss (depilation)
- Skin cell death with scarring (necrosis)
- Reproductive organs
- Infertility
- Lens of the eye
- Whole body radiation damage (only occurs in extremely high radiation exposures beyond those produced by any diagnostic imaging system)
- Bone marrow damage/reduction of blood cell production
- Gastrointestinal mucosa lining loss
- Central nervous system tissue damage
The amount of radiation required to produce these deterministic effects has been derived from studies in experimental cell cultures, animal studies, as well as human epidemiology studies. From these studies, the dose thresholds have been established where the effect is observed in 1% of a population (see Table 1). This means, these values are the amount of radiation energy absorbed by the tissue where if 100 people were exposed to this level of radiation, only a single individual would experience this effect. The unit used for absorbed radiation dose in Table 1 is the Gray (Gy). This value is the standard international measure for absorbed radiation energy. We will see later that this unit must be converted to another unit to understand the stochastic effects (i.e., genetic and cancer effects) of radiation.
Table 1: Dose Threshold for Deterministic Effects* | ||
| Tissue | Total acute dose threshold (Gy) | Time to develop effect |
| Lens of Eye | ||
| Detectable opacities | 0.5–2 | > 1 year |
| Cataract formation | 5.0 | > 1 year |
| Skin | ||
| Skin reddening | 3–6 | 1–4 weeks |
| Temporary hair loss | 4 | 2-3 weeks |
| Skin death and scarring | 5-10 | 1-4 weeks |
| Testes | ||
| Temporary sterility | 0.15 | 3-9 weeks |
| Permanent sterility | 3.5–6 | 3 weeks |
| Ovaries | ||
| Permanent sterility | 2.5–6 | < 1 week |
| Gastrointestinal | ||
| Mucosa lining loss | 6 | 6-9 days |
| Bone Marrow | ||
| Reduction of blood cell production | 0.5 | 1-2 months |
| * 1% incidence level based on ICRP publication 103 (2007) | ||
Reviews of biological and clinical studies have shown that below 0.1 Gy no deterministic effects from radiation exposure have been proven. This is primarily due to the fact that cellular repair mechanisms occur continuously and this prevents deterministic effects at low radiation exposure levels.
The effects from radiation exposures at x-ray energies do not occur during or immediately after the exposure to radiation. This is shown in the column labeled "Time to develop effect" in Table 1. Unlike the exposure to the sun that causes skin reddening within hours of the exposure the effects from these high-absorbed radiation doses require weeks to years following the exposure to produce the effects listed. Therefore, the effect will not be seen at the time of exposure and when the effect does occur the correlation to the radiation exposure may not be easily determined.
A.2. Stochastic Effects (Genetic Changes and Cancer)
Stochastic effects are random or probabilistic in nature. By being random, the occurrence of individual events cannot be predicted. Stochastic effects can be divided into two groups, genetic and carcinogenic effects. Based on the random nature of these effects, the production of genetic changes or induction of cancer in an individual cannot be determined for certain regardless of the amount of energy absorbed; only the probability or the likelihood can be ascertained. As such, there isn't a threshold dose above which these effects will definitely occur. Conversely, there isn't a threshold dose below which the likelihood of these effects could be zero.
Genetic Changes
The exposure to radiation can cause damage in germ cells that ultimately result in mutations in the exposed person's fetus if she is pregnant. But such mutations are not radiation-specific; the radiation only produces DNA sequencing errors that might have occurred naturally. Therefore, instead of producing unique mutations, damage from radiation exposure only results in a higher frequency of normal/spontaneous mutations. This means radiation does not cause the production of monsters as seen in the movies. In addition, a large number of animal and human studies have shown that the adverse effects from radiation exposure are negligible in subsequent generations.
Specifically, there is no direct evidence at any radiation dose that exposure of parents leads to excess genetic disease in their offspring. Therefore, radiation exposure can cause mutations in children if the reproductive cells of the parent are exposed, but the child does not carry any adverse genetic trait produced by the radiation exposure that can be passed on to their offspring. Given these facts, it is very important to inform your physician and the person performing the x-ray study if you are or may be pregnant. As we will discuss later the exposure of a fetus to radiation is a major concern for radiation effects that may occur in a child if the child is exposed before birth.
Cancer Induction
Cancer induction is arguably the most important and the most feared radiation effect. From the discovery of ionizing radiation there has been documented evidence of radiation induced cancer in animal and human studies. The initial human experiences were all at high radiation dose levels from people working with radiation or using radiation without the knowledge of its potential harm. In addition, long-term follow-up studies of the Japanese survivors of the atomic bomb attacks on Hiroshima and Nagasaki and the early medical usage of radiation in treatment and diagnostic studies have shown increased cancer incidence in the exposed populations.
All radiation effects have a latency period between the time of exposure and the onset of the effect, as seen with deterministic effects in Table 1. For cancer induction, the latency period is on the order of years, with leukemia having the shortest latency period (5 to 15 years) and solid tumors having the longest latency period (10 to 60 years). Therefore, it is very difficult to prove that a cancer is directly related to earlier radiation exposure, because other factors encountered during the latency period may be the actual cause of the cancer. This is particularly true when the exposures are at low radiation levels such as those received in diagnostic radiology and cardiology studies.
Currently, at low radiation exposure levels no study has been comprehensive enough to demonstrate stochastic effects conclusively. But as stated above, at very high radiation exposure levels there is good data that proves the induction of cancer from the exposure. So the estimation of risk for cancer induction at low radiation exposure must be extrapolated from the high exposure level data. This is where most of the controversy concerning radiation effects exists. The most conservative estimation of risk from radiation exposure assumes the effects from low radiation exposure are a simple scaled version of the high exposure results (i.e. a linear or straight-line) extrapolation from the high- to the low-exposure results). Most groups that monitor and analyze radiation exposures use this linear extrapolation model to estimate cancer induction from radiation.
Risk Models
Currently there are two models used to assess risk of stochastic effects from radiation exposure; these are the absolute and relative risk models.
Absolute risk is defined as the probability that a person who is disease free at a specific age will develop the disease at a later time following exposure to a risk factor, e.g. the probability of cancer induction following exposure to radiation.
The age-adjusted cancer incidence rate in the United States from 2001 to 2005 was 467 cancers per year per 100,000 men and women
(US Surveillance, Epidemiology and End Results (SEER) Program, see http://seer.cancer.gov)
The relative risk model assumes radiation increases the natural incidence of a cancer and it is expressed as a fraction or multiple of the naturally occurring risk. This value is always greater than 1 (unless the radiation is assumed to produce a beneficial effect – this hypothesis is known as "hormesis" and it will not be considered here). Most advisory publications use the relative risk because it has some mathematical and statistical advantages when derived from epidemiological studies. The current accepted values of relative risk are given in Table 2. Note that a new unit of radiation exposure is used called the Sievert (Sv). This unit is used when defining the effective dose from radiation exposure. It is well known that different tissues react differently to radiation; i.e., some tissues are more sensitive to radiation damage than others. The sensitivity of tissue to radiation is related to the type of radiation (x-rays, alpha particles, etc.) that exposes the tissue and the tissue type that is exposed due to the tissue's cell age, mitotic cycle, and other factors. Therefore, when discussing radiation effects relative to cancer induction, the absorbed radiation energy is normalized to the tissue's sensitivity. This normalization is designated by the use of the Sievert instead of the Gray (the Gray designates the absorbed energy in the tissue only – see Deterministic Effects Section).
Also, when converting the absorbed dose in Gray to the effective dose in Sievert, the geometry of the exposure needs to be known to account for each tissue type that is in the radiation field of view and all tissues that are in or near the radiation field of view that may be exposed to scatter radiation. With the knowledge of what tissue is exposed and the tissue's sensitivity to radiation, there are models based on an average human to determine the conversion factor from Gray to Sievert. Note most imaging studies only involve exposure to a portion of the body, and even so, a fraction of the radiation does not interact with the tissue in the patient at all, but travels through the patient to create the image. Therefore, the conversion from the Gray to Sievert results in each tissue receiving only a fraction of the total energy that entered the patient. The range of values for this conversion is from 1% for radiation-insensitive tissue up to 12% for the most sensitive tissue. Therefore, the effective dose (i.e. Sv) is always less than the absorbed dose (i.e. Gy).
Table 2: Nominal Risk for Cancer Effects* | |
| Exposed population | Excess relative risk of cancer (per Sv) |
| entire population | 5.5% – 6.0% |
| adult only | 4.1% – 4.8% |
| *relative risk values based on ICRP publications 103 (2007) and 60 (1990) | |
Since the results of radiation effects on cell cultures, animal studies, and human epidemiology studies may be interpreted differently, you may see variations in the published relative risk values, but they are all within a few percentage points of each other. Many authors use an average value of 5% per Sievert when discussing the risk of cancer from radiation exposure.
Note that the values in Table 2 are for adults or all people (i.e., entire population). It is known that the sensitivity to radiation varies based on the cell age and mitotic cycle. This suggests that children should have a higher relative risk when compared with adults due to their increased growth rate and ongoing cellular differentiation. This is why there is an increase in the relative risk values for the "entire population" in Table 2. In Figure 2, the estimated lifetime risk that radiation will produce cancer (carcinogenesis) is presented relative to the person's age. This shows that children have a 10% - 15% lifetime risk from radiation exposure while individuals above the age of 60 have minimal to no risk (due to the latency period for cancer and the person's life expectancy).
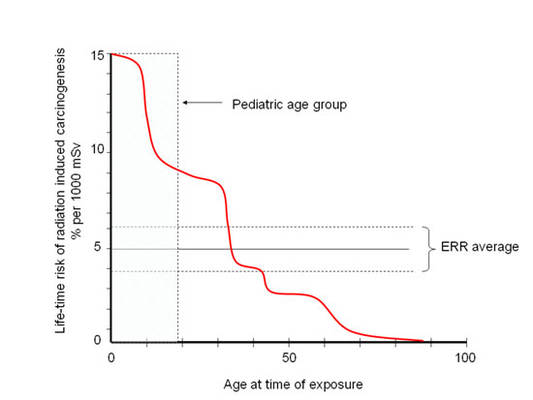
Figure 2 Adapted from ICRP Publication 60 (1990)
These data also demonstrate that you cannot simply use the average relative risk shown in Table 2 to estimate the increased incidence of cancer due to radiation exposure. In order to do this analysis correctly you need take into consideration the age of all individuals in the group that is irradiated.
A.3. Special Considerations for Embryo/Fetus
The early development of life is a time when rapid cell division and differentiation are occurring. Therefore, radiation sensitivity is high for the developing embryo/fetus and protection from radiation needs to be considered differently than the general public. Table 3 provides a review of the stage and deterministic effects that may occur in the embryo/fetus following exposure to different levels of radiation. Similar to what was shown in Table 1, deterministic effects below an absorbed dose of 0.1 Gy are not found, even in the embryo/fetus.
Table 3: Summary of Suspected In-Utero Induced Deterministic Radiation Effects* | |||||
| Menstrual or gestational age | Conception age | <0.05 Gy | 0.05-0.1 Gy | >0.1 Gy | |
| 0 - 2 weeks | Prior to conception | None | None | None | |
| 3rd and 4th weeks | 1st - 2nd weeks | None | Probably none | Possible spontaneous abortion | |
| 5th - 10th weeks | 3rd - 8th weeks | None | Potential effects are scientifically uncertain and probably too subtle to be clinically detectable | Possible malformations increasing in likelihood as dose increases | |
| 11th - 17th weeks | 9th - 15th weeks | None | Potential effects are scientifically uncertain and probably too subtle to be clinically detectable | Increased risk mental retardation or deficits in IQ that increase in frequency and severity with increasing dose | |
| 18th - 27th weeks | 16th - 25th weeks | None | None | IQ deficits not detectable at diagnostic doses | |
| >27 weeks | >25 weeks | None | None | None applicable to diagnostic medicine | |
| *Taken from "ACR Practice Guideline for Imaging Pregnant or Potentially Pregnant Adolescents and Women with Ionizing Radiation", derived from ICRP Publications 84 (2001) and 90 (2004). | |||||
Although deterministic effects are not seen at low dose levels in the embryo/fetus, there have been many studies that have shown an increased incidence of cancer (i.e. stochastic effects) in children following in-utero exposure to radiation. Pre-natal radiation exposures resulted in an increased cancer rate in the offspring of the survivors of the atomic bombings in Hiroshima and Nagasaki. In other epidemiological studies, there have also been good statistical results that demonstrate an increased cancer rate in children following pre-natal radiation exposure from diagnostic radiology studies. Unfortunately, these epidemiological studies do not provide very good data on the specific absorbed dose received to the fetus or embryo. This limits the ability to accurately characterize the dose vs. response as has been done for deterministic effects. But since the doses received in these epidemiology studies were in the diagnostic radiology range, they suggest that low levels of radiation exposure to the embryo/fetus definitely increase the risk of childhood cancer.
B. DOSE METRICS
In the context of dose quantities relevant to the topic of radiation risk, two types of quantities are of importance: dose limits and reference levels. Dose limits refer to the maximum level of dose that the general public can receive from a source other than natural background radiation levels and those received by occupational workers in their job. The reference levels reflect the typical dose values expected in the majority of imaging studies. Both quantities can be described in terms of a number of dose-related metrics, including absorbed dose, effective dose, exposure, or any modality-specific dose index (e.g., CTDI for CT imaging).
B.1. Dose Limits
Limits for exposure to radiation should be at a level below the threshold where deterministic effects occur, i.e. below 0.1 Gy. Furthermore, the limit should exclude exposures from background radiation. Because radiation is around us all of the time from the sun and naturally occurring sources, it would not make sense to try to limit radiation exposure below natural background levels.
As the main concern is stochastic effects, the effective dose with units of Sieverts or 1/1000 of a Sievert (i.e. mSv) is most commonly used. Using the threshold dose as a starting point, dose limits are determined using the Principles of Justification and Optimization.
- Principle of Justification: any decision that alters the radiation exposure to an individual or population should have an outcome that does more good than harm. This means that any radiation source should provide a benefit with its use, either to the individual or to society at large, and the risk of any detrimental effects must be small relative to this benefit.
- Principle of Optimization: the application of radiation in any situation should be developed to minimize the risk of exposure while maximizing the benefit. Overly conservative reduction of radiation exposure from medical procedures may limit the diagnostic quality of the procedure resulting in a reduction in the patient's overall medical outcome. When the medical benefit is retained or maximized, the risk should be as low as possible. The Principle of Optimization is analogous to the As Low As Reasonably Achievable (ALARA) concept.
It is important to understand that dose limits are not levels of exposure that should be considered acceptable in an occupation or that can be safely received by the general public. They are rather maximum limits consistent with the current state of medical practice. In general, the concept of ALARA should still be used when developing radiation protection procedures/policies, and dose limits should be thought of as the maximum exposure that should be allowed in any situation. In most states, the ALARA concept requires investigation into dose-reduction methods even if only a fraction of the limit is received by any individual.
B.2. Reference Levels
The risk and benefit from medical exposures are received by the same individual. Since the individual's situation, body habitus, and medical needs are unique, dose limits do not make sense for medical exposures. Yet an average radiation exposure level received from a diagnostic or interventional procedure can be used to evaluate whether the dose being used for a procedure is within an acceptable range based on existing practice norms. These exposure levels are called reference levels and they are exam-specific.
Reference levels for medical exposures are usually set for an average-size patient at the upper levels (75th percentile) seen in normal practice. The typical operational dose for the majority of exams is expected to be below these values. To make meaningful comparisons, aggregate facility data from average size patients should be compared against benchmark DRLs. If the DRL is exceeded, the protocol should be reviewed to determine methods to reduce the exposure for that exam type at the institution.
Table 4: Diagnostic Exam Reference Levels | |
| Exam | Diagnostic Reference level |
| Radiography | |
| Adult PA chest (23 cm), with grid | 0.15 mGy |
| Pediatric PA chest (12.5 cm), without grid | 0.06 mGy |
| Pediatric PA chest (12.5 cm), with grid | 0.12 mGy |
| Adult AP abdomen (22 cm) | 3.4 mGy |
| Adult AP lumbosacral spine (22 cm) | 4.2 mGy |
| Fluoroscopy | |
| Adult upper GI, without oral contrast media, with grid | 54 mGy/min |
| Adult upper GI, with oral contrast media, with grid | 80 mGy/min |
| Adult film fluorographic PA abdomen, without contrast, with grid | 3.9 mGy |
| Adult digital fluorographic PA abdomen, without contrast, with grid | 1.5 mGy |
| Adult film fluorographic PA abdomen, with contrast, with grid | 27.5 mGy |
| Adult digital fluorographic PA abdomen, with contrast, with grid | 9.9 mGy |
| Computed Tomography | |
| Adult head (16 cm lat), 16 cm CTDI phantom | 75 mGy CTDIvol |
| Adult abdomen-pelvis (38 cm lat), 32 cm CTDI phantom | 25 mGy CTDIvol |
| Adult chest (35 cm lat), 32 cm CTDI phantom | 21 mGy CTDIvol |
| Pediatric (age 5) head (15 cm lat), 16 cm CTDI phantom | 40 mGy CTDIvol |
| Pediatric (age 5) abdomen-pelvis (20 cm lat), 16 cm CTDI phantom | 20 mGy CTDIvol |
| * Taken from ACR-AAPM Practice Guideline Parameter for Diagnostic Reference Levels and Achievable Doses in Medical X-Ray Imaging - Revised 2013 (Res. 47) | |
There are a number of sources for reference level values. Some of these can be found in the Section on Information Sources and Recommended References and Citations. The American College of Radiology (ACR) Appropriateness Criteria® has developed a comparative scale for the Relative Radiation Level (RRL) values based on effective dose (Table 5), which may be used toward reference levels or simple comparison of exams.
Table 5: Relative Radiation Level Scale | ||
| Relative Radiation Level | Effective dose range | Pediatric Effective Dose Estimate Range |
| O | 0 | 0 |
| | Less than 0.1 mSv | Less than 0.03 mSv |
| | 0.1 – 1.0 mSv | 0.03 – 0.3 mSv |
| | 1.0 – 10 mSv | 0.3 – 3.0 mSv |
| | 10 – 30 mSv | 3.0 – 10 mSv |
| | 30 – 100 mSv | 10 – 30 mSv |
| * Adapted from ACR Appropriateness Criteria®, Radiation Dose Assessment Introduction 2016 | ||
Tables 6 – 9 give a sample of the Relative Radiation Level and the range of effective dose values reported for specific diagnostic and interventional radiology examinations. These values are for an average adult patient using typical equipment and techniques. The average effective dose in all of these exams is below 100 mSv (i.e., 0.1 Sv). Therefore, deterministic effects should not be seen for an average patient/exam receiving diagnostic radiology exams. But the potential for stochastic effects must always be considered when an examination is planned.
Table 6: Average Effective Dose in Diagnostic Radiology* | ||
| Exam | Relative Radiation Level | Range of values (mSv) |
| Extremity | | 0.0002 - 0.1 |
| Chest X-ray PA / LAT | | 0.007 - 0.24 |
| Mammography | | 0.1 – 0.6 |
| Abdomen / Pelvis | | 0.04 - 1.2 |
| Thoracic / Lumbar Spine | | 0.5 – 1.8 |
| IVU | | 0.7 – 3.7 |
| Upper GI w/fluoroscopy | | 1.5 - 12 |
| Barium enema w/fluoroscopy | | 2 - 18 |
| *adapted from Mettler FA, et.al. Radiology Vol 248 (1) p254-263 2008 | ||
Table 7: Average Effective Dose in CT* | ||
| Exam | Relative Radiation Level | Range of values (mSv) |
| Head | | 0.9 – 4 |
| Chest (standard) | | 4 – 18 |
| Chest (high resolution, e.g., pulmonary embolism) | | 13 – 40 |
| Abdomen | | 3.5 – 25 |
| Pelvis | | 3.3 – 10 |
| Coronary Angiogram | | 5 – 32 |
| Virtual Colonoscopy | | 4 – 13 |
| Calcium Scoring | | 1 - 12 |
| *adapted from Mettler FA, et.al. Radiology Vol 248 (1) p254-263 2008 | ||
Table 8: Average Effective Dose in Interventional Radiology* | ||
| Exam | Relative Radiation Level | Range of values (mSv) |
| Head/Neck angiography | | 0.8 – 19.6 |
| Coronary angiography (diagnostic) | | 2 – 15.8 |
| Coronary angioplasty, stent placement, RF ablation | | 6.9 – 57 |
| TIPPS | | 20 – 180 |
| *adapted from Mettler FA, et.al. Radiology Vol 248 (1) p254-263 2008 | ||
Table 9: Average Effective Dose in Nuclear Medicine* | ||
| Exam | Relative Radiation Level | Effective dose/ administered activity (mSv/MBq) |
| Brain (Tc99m) | | 0.0093 – 0.0077 |
| Brain PET (18F-FDG) | | 0.019 |
| Thyroid scan (123I) | | 0.075 (w/15% uptake) |
| Thyroid scan (Tc99m) | | 0.013 |
| Cardiac Stress Test (depending on isotope/protocol) | | 0.0085 – 0.22 |
| Cardiac PET (18F-FDG) | | 0.019 |
| Lung Perfusion (Tc99m) | | 0.011 |
| GI Bleed | | 0.007 |
| Renal (depending on isotope/protocol) | | 0.0049 – 0.0088 |
| Bone | | 0.0057 |
| *adapted from Mettler FA, et.al. Radiology Vol 248 (1) p254-263 2008 | ||
C. BALANCING BENEFIT AND RISK
With an understanding of the effects of radiation and the doses for standard examinations, a physician (possibly with the help of a radiologist) can make a determination of which examination provides the most benefit to the patient at the lowest possible dose. To do this, the physician needs consider the following criteria:
- Patient's clinical conditions - What are the benefits of using radiation?
- Availability of equipment - New and changing radiation equipment technology makes the availability of some procedures limited.
- Availability of personnel - Personnel must have the appropriate training on the equipment to perform the procedure desired.
- Alternative exams - All other non-ionizing radiation options (e.g. ultrasound, MRI, EEG, EKG, etc.) for the specific situation cannot provide the desired outcome.
The radiologist and the referring physician ultimately make the choice on which examination to perform, taking into consideration all information known for the specific patient's situation and the imaging options. In general, the use of non-radiation tests should be considered before using radiation, and less invasive procedures should be considered before more invasive techniques are chosen.
The ACR has organized several expert panels to develop criteria for determining appropriate imaging examinations for specific medical conditions. The ACR Appropriateness Criteria® are based on the complexity and severity of a patient's clinical condition and include those exams that are generally used for evaluation of these conditions. All exams that have potential to be used in the specific situation are then ranked based on the appropriateness criteria, taking into account the procedures' risks vs. benefit as defined by the panel of experts. For example, Table 10 shows the Appropriateness Criteria for diagnosing abdominal pain and fever in an adult patient. Table 11 shows an alternate set of criteria if the patient is pregnant.
Table 10: Acute (Nonlocalized) Abdominal Pain and Fever or Suspected Abdominal Abscess | ||
| Exam | Rating 1 = least appropriate 9 = most appropriate | RRL scale |
| CT abdomen and pelvis w/contrast | 8 | |
| CT abdomen and pelvis w/o contrast | 7 | |
| US abdomen | 6 | 0 |
| MRI abdomen and pelvis w/o contrast and w/contrast | 6 | 0 |
| X-ray abdomen | 5 | |
| MRI abdomen and pelvis w/o contrast | 5 | 0 |
| X-ray contrast enema | 4 | |
| Nuclear Imaging Ga-67 of abdomen | 4 | |
| X-ray upper GI series with small bowel follow-through | 4 | |
| CT abdomen and pelvis w/o contrast and w/contrast | 3 | |
| Nuclear Imaging Tc99m WBC abdomen and pelvis | 3 | |
| Nuclear Imaging In-111 WBC abdomen and pelvis | 3 | |
| *adapted from ACR Appropriateness Criteria October 2012. | ||
Table 11: Acute (Nonlocalized) Abdominal Pain and Fever or Suspected Abdominal Abscess | ||
| Exam | Rating 1 = least appropriate 9 = most appropriate | RRL scale |
| US abdomen | 8 | 0 |
| MRI abdomen and pelvis w/o contrast | 7 | 0 |
| CT abdomen and pelvis w/contrast** | 5 | |
| CT abdomen and pelvis w/o contrast | 5 | |
| X-ray abdomen | 4 | |
| CT abdomen and pelvis w/o contrast and w/contrast | 2 | |
| MRI abdomen and pelvis w/o contrast and w/contrast | 2 | 0 |
| X-ray upper GI series with small bowel follow-through | 2 | |
| X-ray contrast enema | 2 | |
| Nuclear Imaging Ga-67 of abdomen | 2 | |
| Nuclear Imaging Tc99m WBC abdomen and pelvis | 2 | |
| Nuclear Imaging In-111 WBC abdomen and pelvis | 2 | |
| *adapted from ACR Appropriateness Criteria October 2012. ** only after other studies without ionizing radiation have been used. | ||
The ACR Appropriateness Criteria® are for generic patient situations and do not take into account secondary conditions the patient may have. For example, it is known that some inherited syndromes (e.g. Down syndrome, Fanconi's anemia, Ataxia-telangiectasia) result in increased sensitivity to radiation. In addition, these criteria assume all equipment options are available at the site.
To get a better understanding of the examination that is being ordered, the ACR and the Radiological Society of North America (RSNA) have established the RadiologyInfo.org website to inform and educate the public about radiologic procedures. This site explains how various X-ray, CT, MRI, ultrasound, radiation therapy, and other procedures are performed. It also addresses what the patient may experience and how to prepare for the exams. The website contains over 100 radiologic procedures and is updated frequently with new information.
Improved awareness and recommendations for imaging pediatric patients has also been initiated by the Image Gently Alliance. This initiative is called the Image Gently campaign. The goal of this campaign is to raise the awareness of radiation dose in imaging children and to suggest methods/processes to provide acceptable images at the lowest doses.
D. PERCEPTION OF RISK
There is risk in all aspects of life and the best that can be hoped for is to minimize the risks that have the greatest potential for disrupting one's life. When a risk has a benefit to an individual or to society the risk may be justified with respect to the benefit. But how can both the risks and the benefits be explained? This requires knowledge of how people perceive risk and how to communicate the risk and the benefit to different populations.
D.1. How to Convey Technical Information to the Public
Medical environments are full of technical jargon that the public and even some personnel within different medical professions cannot understand or interpret correctly. Technical information must be conveyed in simple, clear terms. In addition, care must be taken to emphasize important ideas so that they do not get lost in the discussion. In general the following principles should be used when trying to convey technical information to the public:
- Avoid using technical/medical jargon
- Translate technical/medical terms (e.g., dose) into everyday language
- Write short sentences that convey a single point
- Use headings and other formatting techniques to provide a clear and organized structure to the presentation of information
D.2. Risk Communication vs. Risk Education
Risk communication differs from risk education. When attempting to discuss risk, experts need to understand the value systems of the people they are addressing. This requires an understanding of how different groups may interpret risk.
Individual risk vs population risk
Risk magnitudes and estimates, radiation related or otherwise, are developed based on population statistics. When communicating risk to a patient, we are ascribing the population-base likelihood of harm to an individual, not a population. But in doing so, the risk is not an actual "individual" risk, rather the likelihood of harm to a theoretical population that shares the same attributes as that of the patient, and that one theoretical individual (not necessarily the patient) in that population might be harmed. In this manner, risk is fundamentally a stochastic construct. Without understanding this statistical nature of risk estimates, people tend to use a deterministic interpretation of risk. This often can cause a false understanding of what the risk actually is, especially when compared to other activities or procedures.
Risk ranking
Differences between how scientists and non-scientists rank risk is one of the major problems of risk communication. In general, if scientists and non-scientists are asked to rank a series of health risks the rank orders of the lists are considerably different. This is demonstrated in Table 12 where three different groups were asked to rank 30 activities/sources of risk from the most risky (ranked as 1) to the least risky (ranked at 30). The top 10 risky activities are highlighted. At best, there is a correlation coefficient of 0.6 between the scientific community (i.e. professional society members) and the other groups. At the time this study was conducted, x-ray exposure was ranked 24th by the experts and 17th or 22nd by the other groups. It is clear that different groups will assess risk differently; therefore, we, as the experts, need to understand and address these differences in order to communicate risks and benefits effectively.
Table 12: Perception of Risk* | |||
| Activity (ranked by experts) | League of Women Voters | College students | Professional society members |
| Motor Vehicles | 2 | 5 | 3 |
| Smoking | 4 | 3 | 4 |
| Alcohol | 6 | 7 | 5 |
| Handguns | 3 | 2 | 1 |
| Surgery | 10 | 11 | 9 |
| Motorcycles | 5 | 6 | 2 |
| X-rays | 22 | 17 | 24 |
| Pesticides | 9 | 4 | 15 |
| Electric Power | 18 | 19 | 19 |
| Swimming | 19 | 30 | 17 |
| Contraceptives | 20 | 9 | 22 |
| Private Aviation | 7 | 15 | 11 |
| Large Construction | 12 | 14 | 13 |
| Food Preservatives | 25 | 12 | 28 |
| Bicycles | 16 | 24 | 14 |
| Commercial Aviation | 17 | 16 | 18 |
| Police Work | 8 | 8 | 7 |
| Fire Fighting | 11 | 10 | 6 |
| Railroads | 24 | 23 | 29 |
| Nuclear Power | 1 | 1 | 8 |
| Food Coloring | 26 | 20 | 30 |
| Home Appliances | 29 | 27 | 27 |
| Hunting | 13 | 18 | 10 |
| Antibiotics | 28 | 21 | 26 |
| Vaccinations | 30 | 29 | 29 |
| Spray Cans | 14 | 13 | 23 |
| Football | 23 | 26 | 21 |
| Power mowers | 27 | 28 | 25 |
| Mountain Climbing | 15 | 22 | 12 |
| Skiing | 21 | 25 | 16 |
| *adapted from Slovis P, Science Vol. 236 No. 4799 (1987) | |||
Objective Risks Vs. Subjective Risks
There are two basic translations of how risk is interpreted. These are objective in structure, such as how the scientific community normally interprets risk, and subjective in nature, which is often used by the general public. Objective assessment of risk is what we have done in this document and is based upon peer-reviewed scientific analysis of risks. Yet, the general public may be getting their risk assessment information from less technical sources such as non-peer-reviewed publications and journals (newspapers, magazines, etc.), non-peer-reviewed internet sites (e.g. Wikipedia), non-documentary-based television shows (e.g. Gray's Anatomy, ER), and personal communication in social settings (e.g. discussion with friends). In addition, unlike scientific analysis, the public is unlikely to recall where a fact was presented to them; for instance, they may not be able to recall whether the National Enquirer or the proceedings of the National Academy of Sciences presented the fact. As a result, equal weight may be given to data presented by any source.
The most important point the physician needs to understand is that even though they may know the objective risk of an examination or procedure, they need to be aware of the patients' likely subjective risk assessment during and adjust their conversation accordingly. The methods to do this are educational and motivational rather than scientific.
Furthermore, in medical situations, the patient and their family or friends are often confused and under high stress. In these situations, several things need to be considered:
- People often have difficulty processing information and do not "hear" what is being said to them
- People often become distrustful of anything a person is saying, and therefore do not listen to what is being said
- People often give greater weight to negative information than to positive information
In risk perception theory, perception equals reality. This means there may be no correlation between public perceptions of risk and scientific or technical information. Therefore, discussions of risk should include a sensibility of the likely perception as well as the actual risk. In order to accomplish this, Table 13 offers several fundamental "Do's and Don'ts" for communicating risk.
Table 13: Checklist on Dos and Don'ts When Communicating Risks* | ||
| Category | Dos | Don'ts |
| Truthfulness | Tell the truth | Do not lie or avoid the truth |
| Absolutes | Avoid absolutes --nothing is absolute | Do not use the terms "never" or "always" |
| Jargon | Define all terms and acronyms | Do not use standard medical terminology |
| Negative | Use positive or neutral terms | Do not use negative terms or negative associations |
| Temper | Remain calm | Do not let your feelings interfere with your ability to communicate |
| Clarity | Ask whether you are being understood | Do not assume understanding |
| Abstraction | Use examples, metaphors, and analogies to aid understanding | Do not talk of theoretical concepts without using clear non-technical justification |
| Attack | Only attack the issue | Do not attack the person or organization that may have made incorrect statements |
| Promise | Promise only what you are certain will occur | Do not make promises that you cannot back up and follow through on to ensure they occur |
| Speculation | Provide information only on what is being done and what you know | Do not discuss worst-case scenarios and unintended possible outcomes, unless required by protocol |
| Risk/benefit comparison | Make risk and benefit statements separately | Do not discuss the risk relative to the benefit |
| Risk comparisons | Use tested comparison messages, cite trustworthy data/groups | Do not compare unrelated risks |
| *adapted from EPA Workbook on Risk Communication in Action (2007) | ||
D.4. Risk Comparison
The best practices when making risk comparisons is to use the following criteria:
- Make comparison of the same risk at two different times or circumstances
- Make comparison with a standard that is understood by the listener
- Make comparison with different estimates of the same risk
Often you will read risks compared for unrelated situations. For example, in Table 14 the odds of dying from accidental death are shown. Note the lifetime odds of dying from an injury for a person born in 2005 were 1 in 22 (i.e. 4.5%). This suggests the odds of dying from accidental causes are similar to getting cancer at a later time from an exposure of 1 Sv (see Table 2). The latency is a factor that weights heavily on the risk perception and as such, equal risk factors of different timescale cannot be directly compared. Furthermore, an accidental injury cannot be related to a decision about a medical procedure where the risk of not performing it would have its own associated risk. Herein lies one of the main challenges in communicating risk associated with medical exposures. The exposure involves a finite stochastic risk with a very long latency period but not doing the procedure would have another risk with possibly a much shorter time horizon.
Table 14: Odds of Death From Injury* (Poor comparison for radiation risk) | ||
| Type of incident / Manner of injury | Number of deaths in 2005 | Probability of occurrence |
| All causes of mortality from injuries | 176,406 | 4.5% |
| Transport accidents | 48,441 | 1.3% |
| Automobile | 14,584 | 0.4% |
| Pedestrian | 6,074 | 0.2% |
| Air travel | 590 | 0.02% |
| Non-transportation accidents | 69,368 | 1.8% |
| Falls | 19,656 | 0.5% |
| Being struck by objects | 2,845 | 0.07% |
| Intentional self-harm | 32,637 | 0.9% |
| Assault | 18,124 | 0.5% |
| Complications from medical care | 2,653 | 0.07% |
| *adapted from National Safety Council, http://www.nsc.org/research/odds.aspx | ||
If the issue is primarily communicating the risk of medical radiation alone, a good approach would be to give the risk of exposure to radiation in a radiology exam as an equivalent amount of exposure to the natural background radiation. This is shown in Table 15.
Table 15: Comparison of Adult Exam Dose to Background Radiation Level | |
| Exam | Reference level (time to receive equivalent background radiation) |
| Chest X-ray PA / LAT | 2.4 days / 12 days |
| Mammography | 1 ½ months |
| Abdomen / Pelvis X-ray | 3 months |
| Head CT | 8 months |
| Lung Perfusion (Tc99m) | 8 months |
| Thyroid scan (Tc99m) | 1 ½ years |
| Brain (Tc99m) | 2 years |
| Abdominal CT | 2 ½ years |
| Cardiac Stress Test (depending on isotope/protocol) | 3 years – 13 ½ years |
| Cardiac PET (18F-FDG) | 5 years |
| High resolution Chest CT (e.g. pulmonary embolism, angiogram) | 5 years |
| * Using an average background radiation level of 3 mSv/yr and Tables 8-11 | |
Other comparisons that might be acceptable would be with the estimated risk from cancer induction from naturally occurring or human-induced carcinogens, i.e. radon, arsenic, smoking, etc.
E. BENEFITS VS. RISK OF NOT USING RADIATION
It would be difficult to address all the benefits that are associated with the utilization of radiation in our everyday lives, including its use in medicine. Suffice it to say that radiation is extremely beneficial in many aspects of life when used appropriately. With respect to the use of radiation for diagnosis, assistance in medical interventional procedures, and therapy, the benefits need to be weighed relative to the potential risks. As we have discussed the risk of radiation induced effects are not well understood at the levels of radiation used for diagnostic and interventional procedures. But there are clearly risks associated with not performing an exam that should also be considered.
The risks to consider of NOT performing an exam include missing a diagnosis and/or initiating treatment too late to improve the medical outcome. The potential to reduce a patient's overall life expectancy due to a disease must also be considered in conjunction with the latency period for radiation-induced cancer and the age of the patient.
F. INFORMATION SOURCES
There are many organizations and advisory groups that monitor and assess radiation use and the risks associated with this use. These sources should be considered when developing teaching material or when determining whether radiation information being presented is valid. A brief description of each of these organizations based on their mission statement is given below.
American Association of Physicists in Medicine (AAPM)
Association involved in the advancement of the practice of physics in medicine and biology by encouraging innovative research and development, disseminating scientific and technical information, fostering the education and professional development of medical physicists, and promoting the highest quality medical services for patients.
American College of Radiology (ACR)
A professional society involved in maximizing the value of radiology, radiation oncology, interventional radiology, nuclear medicine, and medical physics by advancing the science of radiology, improving the quality of patient care, positively influencing the socio-economics of the practice of radiology, providing continuing education for radiology and allied health professions, and conducting research for the future of radiology.
Conference of Radiation Control Program Directors (CRCPD)
A non-profit professional organization dedicated to radiation protection and the consistent promotion of methods to resolve radiation protection issues, to encourage high standards of quality in radiation protection programs, and to provide leadership in radiation safety and education.
International Commission on Radiation Protection (ICRP)
An independent registered charity established to advance for the public benefit the science of radiological protection, in particular by providing recommendations and guidance on all aspects of protection against ionizing radiation.
National Council on Radiation Protection and Measurements (NCRP)
Chartered by the U.S. Congress to collect, analyze, develop, and disseminate in the public interest information and recommendations about protection against radiation and radiation measurements, quantities and units, particularly those concerned with radiation protection.
National Research Council (NRC) of The National Academies of Sciences (NAS)
A private, nonprofit institution that provides science, technology, and health policy advice to governments.
See Biological Effects of Ionizing Radiation Reports (e.g. BEIR VII Phase 2).
Nationwide Evaluation of X-ray Trends (NEXT)
Joint effort of the FDA Center for Devices and Radiological Health (CDRH) and the Conference of Radiation Control Program Directors (CRCPD) to characterize the radiation doses patients receive and to document the state of the practice of diagnostic radiology.
Radiological Society of North America (RSNA)
A professional society involved in promoting and developing the highest standards of radiology and related sciences through education and research. The Society seeks to provide radiologists and allied health scientists with educational programs and materials of the highest quality, and to constantly improve the content and value of these educational activities.
See www.radiologyinfo.org website designed for the general public to answer questions related to the many radiologic procedures and therapies.
Society of Pediatric Radiology
The Image Gently Alliance, i.e. Image Gently campaign
Alliance of organizations and people with a goal to change the practice of imaging children through increasing awareness of the opportunities to lower radiation dose in imaging. The Alliance began as a Committee within the Society for Pediatric Radiology.
United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR)
Established by the General Assembly of the United Nations to assess and report levels and effects of exposure to ionizing radiation.
Center for Devices and Radiological Health (CDRH)
Component of the U.S. Food and Drug Administration (FDA) that provides independent, professional expertise and technical assistance on the development, safety and effectiveness, and regulation of medical devices and electronic products that produce radiation.
U.S. Surveillance, Epidemiology and End Results Program (SEER)
An adjunct to the National Cancer Institute that is a source for cancer statistics in the United States.
G. RECOMMENDED REFERENCES AND CITATIONS
- ACR-SPR Practice Guideline Parameter for Imaging Pregnant of Potentially Pregnant Adolescents and Women with Ionizing Radiation
https://www.acr.org/-/media/ACR/Files/Practice-Parameters/Pregnant-Pts.pdf. - ACR-AAPM-SPR Practice Parameter for Diagnostic Reference Levels and Achievable Doses in Medical X-Ray Imaging https://www.acr.org/-/media/ACR/Files/Practice-Parameters/Diag-Ref-Levels.pdf.
- ACR Appropriateness Criteria® Radiation Dose Assessment Introduction (2016) https://www.acr.org/-/media/ACR/Files/Appropriateness-Criteria/RadiationDoseAssessmentIntro.pdf.
- Broadbent MV, Hubbard LB. Science and perception of radiation risk. Radiographics 1992; 12: 381-392.
- Gail MH. Models of absolute risk, use, estimation and validation, Chapter 11, Cancer Chemoprevention, Volume 2: Strategies for Cancer Chemoprevention, edited by Kelloff GJ, Hawk ET, Sigman CC, Humana Press, Totowa, NJ, 2005.
- Hall EJ, Garcia AJ, Radiobiology for the Radiologist, 6th Ed, Lippincott Publishing, 2006.
- Hendee WR, Personal and public perceptions of radiation risk. Radiographics 1991; 11: 1109-1119.
- ICRP 103 Recommendations of the ICRP, Vol 37 (2-4), 2007.
- ICRP 60 Recommendations of the ICRP, Vol 21 (1-3), 1991.
- ICRP 84 Pregnancy and Medical Radiation, Vol 30 (1), 2001.
- ICRP 90 Biological Effects After Prenatal Irradiation (Embryo and Fetus), Vol 33 (1-2), 2003.
- ICRP 99 Low-Dose Extrapolation of Radiation-Related Cancer Risk, Vol 35 (4), 2005.
- ICRP 105 Radiological Protection in Medicine, Vol 37 (6), 2007.
- ISO 14971: 2007. Medical devices—Risk management—Application of risk management to medical devices.
- Kaste SC. Imaging challenges: a US perspective on controlling exposure to ionizing radiation in children with cancer. Pediatric Radiology 2009; 39 Suppl 1: S74-S79.
- Kleinerman RA. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2656401/, Pediatric Radiology 2009; 39 Suppl 1: S27-S31.
- Kuhn JP, Slovis TL, Haller JO. Caffey's Pediatric Diagnostic Imaging, 10th Ed, Mosby Publishing, 2003
- Kuperman VY. General properties of different models used to predict normal tissue complications due to radiation. Med Phy 2008; 35(11): 4831-4836.
- Linet MS, Kim KP, Rajaraman P. Children's exposure to diagnostic medical radiation and cancer risk: epidemiologic and dosimetric considerations. Pediatric Radiology 2009; 39 Suppl 1: S4-S26.
- Little MP, Muirhead CR. Absence of evidence for threshold departures from linear-quadratic curvature in the Japanese A-bomb cancer incidence and mortality data. Int J Low Radiat 2004; 1: 242-255.
- Little MP, Muirhead CR. Curvature in the cancer mortality dose response in Japanese atomic bomb survivors: absence of evidence of threshold. Int J Radiat Biol 1998; 74: 471-480.
- Little MP, Muirhead CR, Evidence for curvilinearity in the cancer incidence dose-response in the Japanese atomic bomb survivors. Int J Radiat Biol 1996; 70: 83-94.
- Little MP, Muirhead CR, Charles MW. Describing time and age variations in the risk of radiation–induced solid tumour incidence in the Japanese atomic bomb survivors using generalized relative and absolute models. Statistics in Medicine 1999; 18(1): 17-33.
- Mettler FA, Huda W, Yoshizumi TT, Mahesh M. Effective dose in radiology and diagnostic nuclear medicine. Radiology 2008; 248(1): 254-263.
- NCRP Report 116 Limitation of Exposure to Ionizing Radiation, National Council on Radiation Protection and Measurements, Bethesda, MD, 1993
- National Research Council, Health Risks from Exposure to low levels of Ionizing Radiation, BEIR VII Phase 2. National Academies Press 2006.
- Patel SJ, Reede DL, Katz DS, et al. Imaging the pregnant patient for non-obstetric conditions: Algorithms for radiation dose considerations. Radiographics 2007; 27(6): 1705-1722.
- Paterson A, Frush DP. Dose reduction in paediatric MDCT: general principles. Clinical Radiology 2007; 62(6): 507-517.
- Pierce DA, Preston DL. Radiation-related cancer risks at low doses among atomic bomb survivors. Radiat Res 2000; 154(2), 178-186.
- Reckelhoff-Dangel C, Peterson D. EPA Risk Communication in Action, The Risk Communication Workbook. Office of Research and Development EPA/525/R-05/003, 2007
- Slovis P. Perception of risk. Science 1987; 236 (4799): 280-285.
- Vaeth M, Pierce DA. Calculating Excess Lifetime Risk in Relative Risk Models. Environmental Health Perspectives 1990; 87: 83-94.
- Verdun FR, Bochud F, Gudinchet F, et al. Quality initiatives radiation risk: What you should know to tell your patient. Radiographics 2008. 28(7); 1807-1816.
Chapter 31 Review Answers Principles of Radiographic Imaging 6th Edition
Source: https://www.imagewisely.org/Imaging-Modalities/Computed-Tomography/How-to-Understand-and-Communicate-Radiation-Risk